When immune responses are directed toward the brain
Treatment resistant symptoms
The role of immune dysfunction
Immune dysfunction is a well-established factor in the development of psychiatric disorders. Recent research suggests that, in the context of COVID-19, cognitive, emotional, and behavioural symptoms may result from infection-induced immune changes affecting the brain. Studies conducted by the National Institutes of Health have also linked brain inflammation caused by COVID-19 to the mood and cognitive symptoms observed in patients experiencing long-COVID.

Take charge of your journey
Innovative testing to uncover hidden causes
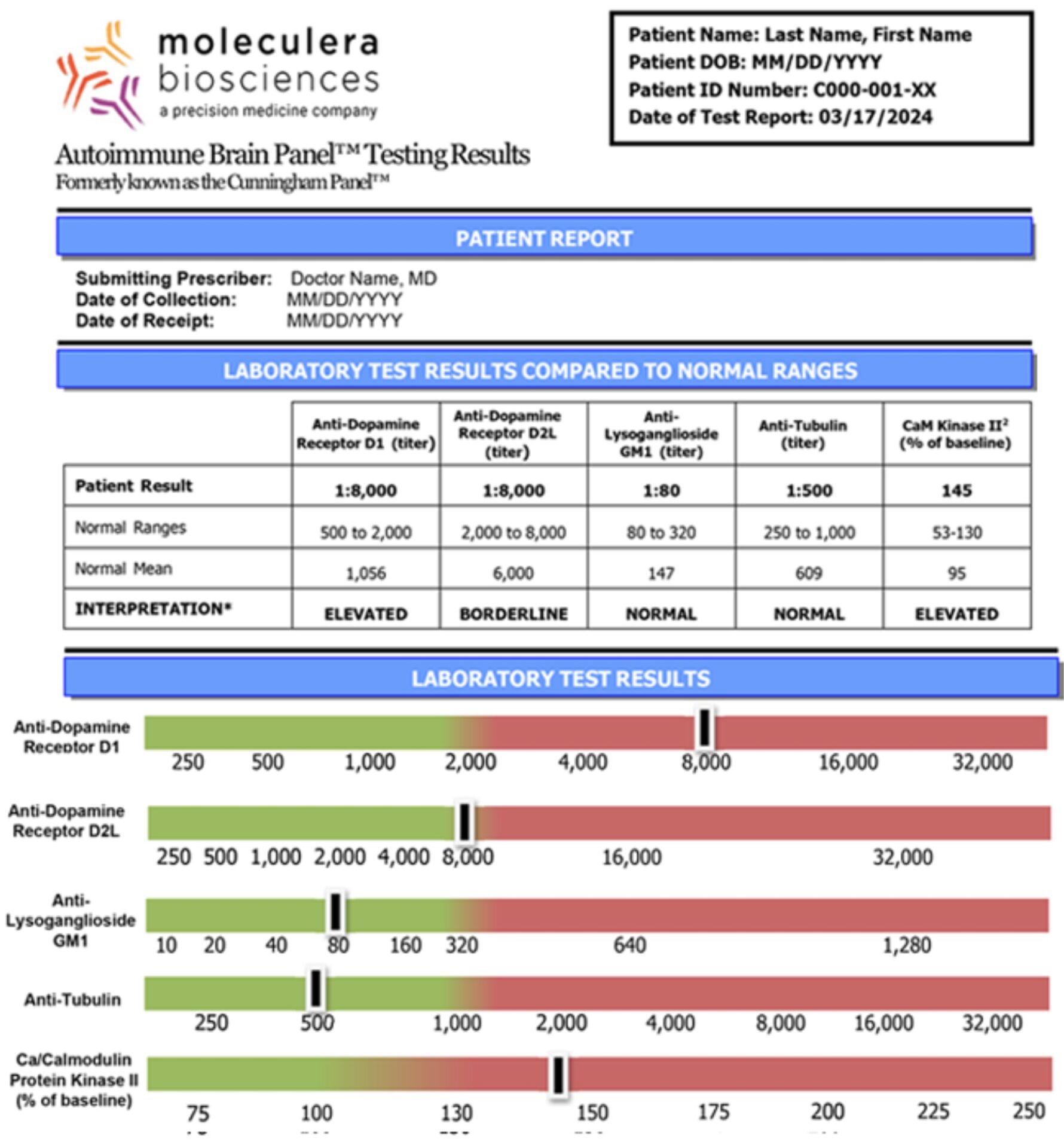
If medications, therapy, or other treatments have not been effective in addressing your symptoms, there is still hope. The Autoimmune Brain Panel™ is a unique testing tool that helps identify whether neurological or psychiatric symptoms may be linked to an underlying autoimmune disorder. Identifying an autoimmune condition is crucial because therapies target the underlying infections and regulates the immune system, rather than relying solely on psychotropic medications. With appropriate therapies, symptoms can be significantly improved or fully resolved.
Case Study: A Schizophrenia Diagnosis Reevaluated
A 15-year-old girl presented with multiple neuropsychiatric symptoms that were unresponsive to various treatments, leading to four hospitalisations. Initially diagnosed with schizophrenia, further testing with the Autoimmune Brain Panel™ revealed that her symptoms were caused by an underlying autoimmune process rather than a primary psychiatric disorder.
Resolution of symptoms
Testing with the Autoimmune Brain Panel™ (formerly the Cunningham Panel™) identified elevated autoimmune antibody levels, indicating an autoimmune origin for her symptoms. Following appropriate immunomodulatory therapy, she experienced complete resolution of symptoms.
60% of patients with neuropsychiatric and behavioral disorders don’t respond to treatment.
Autoimmune Brain Panel™
Discoveries that bring clarity and direction
Who can benefit from the Autoimmune Brain Panel™?


Why is the Autoimmune Brain Panel™ vital?
Refrences:
Howes, O. D., et al. (2022). “Treatment resistance in psychiatry: state of the art and new directions.” Mol Psychiatry 27(1): 58-72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8960394/
Bower JE, Radin A, Kuhlman KR. Psychoneuroimmunology in the time of COVID-19: why neuro-immune interactions matter for mental and physical health. Behav Res Ther. 2022;154:104104. doi:10.1016/j.brat.2022.104104. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9075982/
Inflammation pattern in the brain may cause many long COVID symptoms. National Institutes of Health. Updated November 8, 2022. Accessed November 20, 2022. https://covid19.nih.gov/news-and-stories/inflammation-pattern-brain-may-cause-many-long-covid-symptoms
Drew H. Barzman, Hannah Jackson, Umesh Singh, Marcus Griffey, Michael Sorter, and Jonathan A. Bernstein, “An Atypical Presentation of Pediatric Acute Neuropsychiatric Syndrome Responding to Plasmapheresis Treatment,” Case Reports in Psychiatry, June 28, 2018, Vol. 2018, doi.org/10.1155/2018/8189067. https://www.hindawi.com/journals/crips/2018/8189067/
Shin Y-W, Lee S-T, Park K-I, et al. Treatment strategies for autoimmune encephalitis. Therapeutic Advances in Neurological Disorders. January 2018. doi:10.1177/1756285617722347. https://pubmed.ncbi.nlm.nih.gov/29399043/
Brenton JN, Goodkin HP. Antibody-Mediated Autoimmune Encephalitis in Childhood. Pediatr Neurol. 2016 Jul;60:13-23. doi: 10.1016/j.pediatrneurol.2016.04.004. Epub 2016 Apr 12. PMID: 27343023. https://pubmed.ncbi.nlm.nih.gov/27343023/

